If you’re suffering from a chronic or acute cardiac condition, or recovering from cardiac surgery, your healthcare provider may refer you for cardiac rehabilitation. Cardiac rehab has been proven to have significant benefits for patients: it can improve your quality of life, help you manage or reduce cardiac symptoms, and even lengthen your life.
In this article, we’ll break down the four stages of cardiac rehabilitation—also known as the acute, subacute, outpatient, and maintenance phases. We’ll guide you through what happens at each stage and look at potential benefits and goals you can aim for, as you move through your recovery from a cardiac event or condition.
What is Cardiac Rehab?
Cardiac rehab is a comprehensive, medically supervised recovery program, specifically designed for patients with heart disease. Typically, a cardiac rehab program will begin with a careful analysis of a patient's condition and needs, followed by a supervised, progressive exercise regime, combined with education on a heart-healthy lifestyle and medications. Cardiac rehab may be beneficial for patients with any kind of heart condition, including coronary artery disease, angina, heart failure, heart attack, or heart surgery.
A cardiac rehabilitation program will likely progress through the four main phases:
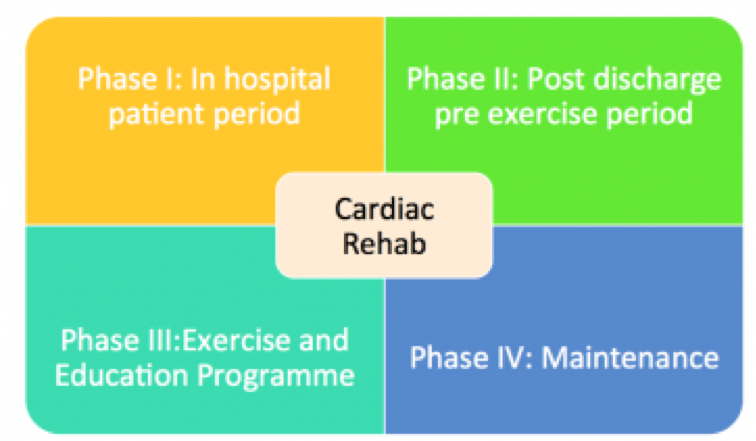
Phase 1: Acute, In Hospital Patient Period
Patients with acute heart conditions, such as those recovering from heart surgery or a heart attack, may be referred to a cardiac rehab team while still in hospital. This phase will likely last between two and five days, depending on your physical condition.
What happens in phase 1 of cardiac rehab?
1. Assessment
During this phase, you will be visited by cardiac rehab specialists, who will begin by providing you with support and information as you begin recovery. Your cardiac rehab team may run the following tests:
- Heart rate
- Blood pressure
- Oxygen saturation
- Upper extremity function, including strength and range of motion (ROM)
- Lower extremity strength
- Functional mobility such as walking and self-care tasks
They will also take a full medical history, to identify any particular risk areas or comorbidities (other diseases that might complicate your recovery).
2. Education
You may begin to receive education and training on:
- The cardiac event itself
- Specific aspects of your diagnosis and condition
- Managing your psychological reactions to the event
- Managing cardiac pain or other symptoms
- Monitoring
You will be closely monitored to make sure that you don’t experience any worsening of your symptoms or risk another cardiac event.
3. Physical Therapy
You may be assigned an acute care physical therapist, who will design a carefully monitored, progressive, and very limited exercise program to get you back on your feet again. This might involve initially just sitting up in bed, standing and testing your range of motion, before moving to short walks around the hospital wing.
4. Discharge Plan
Your cardiac rehab team will also be able to provide you with a plan for leaving the hospital. They will assess your ability to walk, your need for home oxygen, and assess any additional training or medical needs you may have before you leave. They may also work with your family or loved ones to ensure you have adequate care and support when you are discharged.
Goals for Phase 1:
The main goal for the first phase of cardiac rehabilitation is to enable you to leave the hospital and return home as quickly and safely as possible. You will work with doctors, nurses, and physical therapists or other specialists to design a safe and appropriate discharge plan. By the end of this phase, you should have:
- A safe, limited exercise plan that you can follow at home
- A clear understanding of your condition and your cardiac rehabilitation program
- Knowledge about self-care for your wounds (if you have had open heart surgery)
- An assistive device, such as a cane or walker, if needed
- Access to home oxygen therapy, if needed
By the end of Phase 1, you should have recovered sufficiently to return home and begin the second phase of cardiac rehab.
Phase 2: Subacute Outpatient Care (Post-discharge, Pre-Exercise Period)
Phase 2 takes place after you leave the hospital, at an outpatient care facility. This second phase will last between three and six weeks.
What happens in phase 2 of cardiac rehab?
The primary focus of this phase is close monitoring to ensure that you are progressing in your recovery. You will also receive more extensive training on how to manage your condition. Your cardiac rehab team will review how your heart responds to gradually increasing levels of exercise and activity. You will receive guidance on how to use your medication and how to reduce the risk of cardiac events. During this stage, the aim is to reach a point at which you are able to exercise and begin your journey to full recovery.
Goals for Phase 2:
1. Reinforce learning from Phase 1
The main goal for Phase 2 is to support your learning from Phase 1—and ensure that you have taken all the new information on board. You will be monitored as you make any necessary lifestyle changes and begin to progress with your exercise regime.
2. Move toward independent self-care
The other key aspect of this second phase of cardiac rehab is to help you become more independent and informed. You should learn how to self-monitor your heart rate and exertion levels during exercise. The main goal is to increase your levels of independence and enable you to move into Phase 3.
Phase 3: Intensive Outpatient Rehab
If you have experienced a severe cardiac event or surgery, you will probably need to complete phases 1 and 2 before you are moved into Phase 3, a full cardiac rehabilitation program. Some patients with less intense cardiac conditions may enter Phase 3 directly. Phase 2 is very closely supervised and is aimed at patients who are still very severely affected by their heart condition, whereas Phase 3 introduces more independent exercises and self-monitoring.
According to VeryWell Health, “You are usually ready to start phase 3 cardiac rehab when your vital signs, such as heart rate and blood pressure, remain stable as you increase your activity and workloads prescribed in the sub-acute phase of cardiac rehab.”
Typically, a full Phase 3 cardiac exercise and training rehab program will comprise 36 outpatient sessions, although some patients may need inpatient care and others may need fewer sessions and/or less supervision. This stage is often covered by health insurance.
What happens in phase 3 of cardiac rehab?
A team of cardiac rehab specialists, including doctors, nurses, physiotherapists, and nutritionists, will put together an individualized treatment plan, customized to your unique combination of symptoms and current physical condition. The rehab program at this stage will involve close assessment and monitoring, exercise, and further training.
Exercise
During cardiac rehab, your exercise program will be closely supervised by medical professionals to ensure your safety. Your level of exercise will depend on how fit you were before your cardiac condition, your current stamina and ability, your symptoms, and a number of other health factors.
A physical therapist will evaluate you before you begin, taking careful note of your range of motion, muscle strength, resting heart rate, blood pressure, respiration, endurance levels, and any issues with scar mobility if you have had surgery. Your cardiac rehab exercise sessions will usually include a warm-up, cardiovascular exercise (such as the use of a stationary bike or treadmill), and cool down. Depending on your physical condition, you may also be advised to include some resistance training. You will be encouraged to monitor your own response to exercise, including your heart rate, level of exertion, and blood pressure.
Education
During this phase, it’s important to ensure you have all the information you need to maximize your quality of life, manage your symptoms, and feel confident that you can look after yourself despite your heart condition. Training at this stage will probably focus on:
1. Nutrition
Eating a heart-healthy diet is critically important for patients with cardiovascular conditions. You will also need to aim to maintain a healthy weight to avoid putting undue strain on your heart. You will probably be provided with a diet plan by your cardiac rehab team. Generally, a diet that promotes heart health will be low in salt, sugar and trans fats, and include fruits and vegetables, whole grains, and lean proteins.
2. Lifestyle
Long-term quality of life with a heart condition may require you to make changes to your lifestyle—for instance, by quitting smoking and exercising regularly. During Phase 3 of your cardiac rehab program, your team of rehab specialists will help support you as you make any necessary changes and provide you with guidance and advice on how to make these changes permanent.
3. Stress Management
It is very important to learn how to manage stress well if you suffer from a heart condition. Your cardiac rehab program may well include stress management training, such as breathing techniques and meditation, to help you keep your stress levels down once rehab finishes. You may also receive counseling to help address any underlying factors that could be creating anxiety.
Goals for Phase 3:
The main goal for Phase 3 of cardiac rehab is to give you the tools to manage your heart condition on your own and live a longer, happier and healthier life.
When you complete your rehab program, you should have a clear idea of how to manage your symptoms, deal with chest pain, keep an eye on your blood pressure and exertion levels, and control your own medications, oxygen, and other treatments.
You should also have a good understanding of the elements of a heart-healthy lifestyle, including how to exercise safely, eat well, and manage your stress levels. Hopefully, you will have successfully stopped smoking and made any necessary lifestyle changes to promote your overall well-being. Ideally, you will be experiencing fewer symptoms from your heart condition and be less likely to have a second event or need to return to the hospital.
Phase 4: Maintenance
If you have completed the previous three stages of cardiac rehabilitation, you should have a clear grasp of your heart condition and how best to manage it. Phase 4 essentially continues for the rest of your life.
What happens in phase 4 of cardiac rehab?
During Phase 4, you should continue to follow the guidance on exercise, nutrition, and lifestyle, as set out by your rehab team. You may proceed independently, or you may decide to self-fund further training with a physical therapist to help support you as you progress. There are also qualified gym instructors who can offer ongoing exercise training. You should receive regular check-ups with your healthcare provider to make sure that you are effectively managing your heart condition and avoid any flare-ups.
Goals of Phase 4
The goal of Phase 4 is to continue to maintain the changes to your lifestyle that you instigated in Phase 3, keep up with your exercise regime, continue to avoid tobacco, eat well, and manage your stress.
At Rehab Select, we offer specialized cardiac rehabilitation in Alabama for both acute and chronic heart conditions. Our experienced staff can guide you through the phases of cardiac rehab at one of our five Alabama locations with a personalized, physician-led program to improve your heart health and quality of life. To find out more about cardiac care at Rehab Select, please click here or contact us for more information.